An effective team is now globally recognized as an essential tool for constructing a more effective and patient-centred health care delivery system. Identifying best practices through rigorous research, which can provide data on optimal processes for team-based care, is subject to identification of the core elements of this system.
High-functioning health care teams can enhance medical education and improve outcomes. And they help team members feel invested in their work. Poorly functioning teams often achieve the opposite. Numerous peer-reviewed studies show that group dysfunction leads to burnout, emotional distress, depression, substance abuse, reduced productivity, and other psychosocial issues.
Improved Patient Responsiveness
Health care providers working as a team can be more responsive to changes as they occur. When a patient’s condition worsens, the team looks to the leader, knowing that everyone on the team will carry out their respective duties and work with others to solve problems. Trust develops in a cohesive team, increasing confidence in your partners, knowing they will fulfill their duties during a crisis. Nurses, doctors and assistants working as a team tend to make fewer mistakes, leading to improved patient outcomes.
Overall Satisfaction
Patients are more satisfied with their care when health care professionals collaborate. The health care team and the patients experience less stress when members of the team fulfill their duties, knowing their counterparts are working toward coordinated goals. When the roles are clear among team members, there is less confusion about patients’ treatment plans. Simultaneously, when communication is clear among the team, patients also experience greater clarity about their treatment and expected outcome.
“Health care is a high-stress environment that requires a lot of people from different perspectives to work together,” said Michael Leiter, PhD, an organizational psychologist and professor at Acadia University in Wolfville, Nova Scotia. “When communication and cooperation unravel among a group of health care providers, patient care suffers.”
“It’s when people understand their roles, feel like their contributions are valued, and have a sense of belonging that we can deliver patient care in the most optimal way.”
Brenessa Lindeman, MD, MEHP
The importance of social dynamics
Leiter and experts such as Christina Maslach, PhD, an authority on workplace burnout and professor of psychology at the University of California, Berkley, met at Georgetown University Medical Center in October 2015 for the CENTILE International Conference to Promote Resilience, Empathy, and Well-Being in Health Care Professions. A major area of focus at the conference was the importance of social dynamics in medical education and health care delivery.
Maslach has been investigating the interplay of social relationships in the workplace since 1971 and created the Maslach Burnout Inventory, the most widely used instrument for assessing burnout today.
“The people you work with are the people who can understand you the best and be the best source of support, but they also have the power to make your life miserable; what people refer to as a socially toxic workplace,” Maslach said. “So the quality of those social relationships and how to make them function as positively as possible is really critical in terms of making things go well or badly.”
Workplace harmony hinges on community, she explained, and if the community is weak and colleagues are unsupportive—or engage in incivility and bullying—it is difficult to resolve conflict and the team suffers.
Improved Efficiency
Teams that are highly involved in treatment plans and service delivery tend to be more efficient and utilize resources better. When health care providers adopt the team approach to medical care, mirroring the success achieved in other industries that employ teamwork techniques, facilities become more competitive and save money. With strong team leadership, efficiency is realized even more when health care teams are empowered to design their work plans according to their skills and resources.
Increased Effectiveness
Your education teaches you about your special area of work but you often know little about what other providers bring to the complete treatment plans of patients. You need to understand the duties of each team member to work together effectively, increasing your own skills as duties often overlap. As part of the team, you come to understand and appreciate the roles of physicians, nurses, nursing assistants, social workers, physical therapists and administrators as you communicate and work together in the best interests of the patient.
Civility, respect, and engagement
Communication is essential to resolving conflict, said Maslach, but often there is a lack of training to address matters such as, “How do we talk to each other? How do we raise issues? How do we solve conflicts? How do you build trust and support so that if something goes wrong, people don’t hide it or fail to resolve it or get worried that they’ll get in trouble, but instead actually work together to get it solved?”
At the Geisel School of Medicine at Dartmouth, Catherine F. Pipas, MD, MPH, assistant dean for medical education and professor of community and family medicine, teaches courses on team improvement. First-year medical students are broken into groups of four and five within their anatomy teams. Each group tracks the team’s collective vision, goals, and role assignments, in addition to how individual team members are progressing in terms of authenticity and resilience.
“We are all at risk for many, many reasons,” said Pipas. “We are in a health care field where we are constantly giving. We lack control, have a heavy workload, and have increased autonomy—all factors that put one at risk for burnout. So, it’s important that we have trusted relationships so we can depend on others to look at us and say ‘You are not performing’ or ‘We are seeing some change in your patterns; what’s going on and how can we help?’”
For all the hard work to improve coordination and collaboration in health care, most hospitals are still organized into silos based on clinical specialties — and communication among them is uneven at best. Teams may function fairly well within silos, but coordination across them is often poor, which has potentially serious consequences for patients.
The solution to these problems is to shift focus from the structure to the activities of teamwork — what can be called “teaming.” Teaming involves fluid, collaborative, interdependent work across shifting projects and with a shifting mix of partners, often across organizational boundaries.
Few industries present more teaming opportunities — or have a greater need for it — than health care. Why?
Patient-care tasks require the real-time integration of diverse skills and expertise, and the 24/7 operations of hospitals and other clinical delivery systems require sophisticated coordination across shifts. This can increase throughput time from the desired couple of hours to a full day, and sometimes even longer.
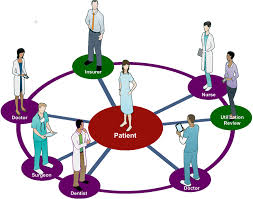
Putting patients needs first and allowing them to be the focal point and at the center of the team will foster a better patient relationship and better outcomes. By being empathetic, listening and communicating and understanding that patients are the most important part of the team; health care professionals can create a treatment plan that correlates with patients needs. Every patient is the most important member of the health care team.
Your turn
We would love to hear your insightful thoughts. Do you feel that you are the most important part of the medical (health care team)? What are your experiences? Do you consider yourself an empowered patient? Do you take charge of your health? Have there been times when you were afraid to speak up? Are you involved in the decision making process with your health care professionals?

Recent Comments