The typical nurse’s day is active and multi-faceted. A nurse may walk up to five miles in a ten-hour shift (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3037121/), all the while facing fluctuating conditions throughout his or her workflow: collaborating with doctors and therapists, consulting with patients, attending to and working around patient families, and interacting with other hospital staff. Nurses navigate these waters on a daily basis, and not surprisingly, this busy environment is not always conducive to supporting caregiver health, resulting in discomfort and injury.
As the healthcare system in the United States continues its digital transformation to improve patient and caregiver health, the nursing population finds itself stuck between two worlds. Nurses remain mired in legacy burdens of the job and now face new challenges as a result of the massive electronic health record (EHR) restructuring.
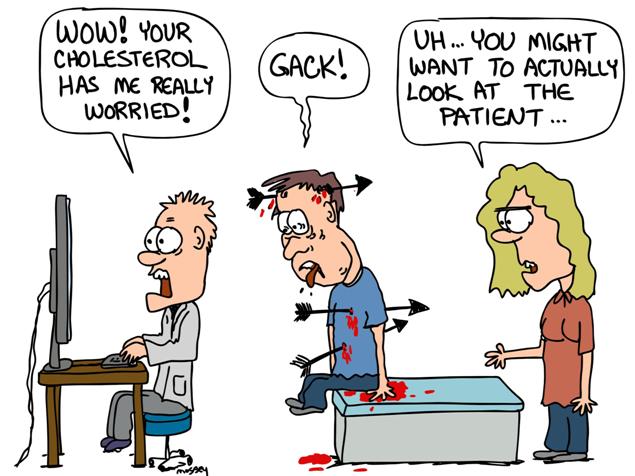
Electronic healthcare records (EHRs) are designed to streamline patient information delivery and caregivers’ access to it throughout their digital workflow, helping to improve documentation processes and hopefully improve patient care. But a number of factors—from the type of system deployed to the position and ease of use of the equipment—may be negatively impacting nurses, including increasing the level of stress on the job.
The first national coordinator for health information technology, Dr. David J. Brailer, was appointed in 2004, by President George W. Bush. Dr. Brailer encouraged the beginnings of the switch from paper charts to computers. Dr Brailer explained that the current information tools are still difficult to set up. They are hard to use. They fit only parts of what doctors and nurses do, and not the rest.
How much has changed in 12 years ?
There is longstanding evidence that linkages exist between nursing care and improved patient outcomes. Florence Nightingale used quality improvement data and statistics to support a hand washing campaign that prevented soldiers from dying of hospital acquired infections during the Crimean war (Gill & Gill, 2005). Over the past decade, the Robert Wood Johnson Foundation’s Interdisciplinary Nursing Quality Research Initiative demonstrated the impact of nursing care on patient sensitive outcomes, such as fall prevention.
Clinical data that is necessary to represent nursing care processes and associated outcomes are not consistently documented in the electronic record. When nurses do document interventions intended to improve patient outcomes, it may not be in a format that supports secondary use (e.g., free-text data or uncoded structured data). Workflow barriers exist to capturing clinical data at the point of care in an interoperable format.
Data is needed to represent the structure, process, and outcomes of nursing care. Mobile solutions that support nursing workflow, nursing movement and understanding of priorities and decisions at the point of care is the first step in the behavior needed to capture the data necessary to improve patient outcomes and improve quality care.
Workflow inefficiencies reduce the time needed to perform critical tasks, creating an environment susceptible to errors. Inefficiencies are partially driven by the design and layout of commonly used areas and items. New system and device implementation provides an organic opportunity to evaluate and design a more efficient process that supports success in nursing practice.
The design of good organizational workflow is not simply about improving efficiency. Workflow processes are maps that direct the care team how to accomplish a goal. A good workflow will help accomplish those goals in a timely manner, leading to care that is delivered more consistently, reliably, safely, and in compliance with standards of practice. An excellent workflow process can accommodate variations that inevitably arise in health care through interaction with other workflow processes, as well as environmental factors such as workload, staff schedules, and patient load.
Workflow design is a difficult endeavor because of the complexity of most health care organizations and the division of labor into expert roles. Health care organizations are service organizations that are very flexible and interdependent in response to dynamic patient needs. For many work processes, the established workflow evolved over time in response to the kind of tasks and resources available, and were not explicitly considered or designed. Changes to organizational workflow are an opportunity to think through how the care team can provide good patient care reliably under a variety of circumstances.
Brenda Hopkins RN, MBA

Recent Comments